While the American food supply is among the safest in the world, the CDC estimates that there are about 48 million cases of foodborne illness annually – that’s 1 in 6 Americans each year. And each year these illnesses also result in an estimated 128,000 hospitalizations and 3,000 deaths.
Food Illness threats are numerous and varied, with symptoms ranging from relatively mild discomfort to very serious, life-threatening illness. While the very young, the elderly, and persons with weakened immune systems are at greatest risk of serious consequences from most foodborne illnesses
 Image Source: Shutterstock
Image Source: Shutterstock What is Foodborne Illness?
Foodborne illness (also referred to as food illness, food poisoning, and foodborne disease) is mostly caused by pathogens – bacteria, viruses, or parasites (also referred to as biological hazards).
But, some cases of foodborne illness can be linked to either natural toxins or chemical contaminants (also referred to as chemical hazards). Likewise, food allergens are a chemical hazard in the natural toxin sub-category.
Physical hazards such as glass, metal, dirt, hair, droppings from pests can also cause foodborne illness. Furthermore, some physical contaminants can be biologically contaminated.
Understanding the causes, signs and symptoms, and vulnerable groups of foodborne illness is essential to keep food safe to prevent food poisoning.
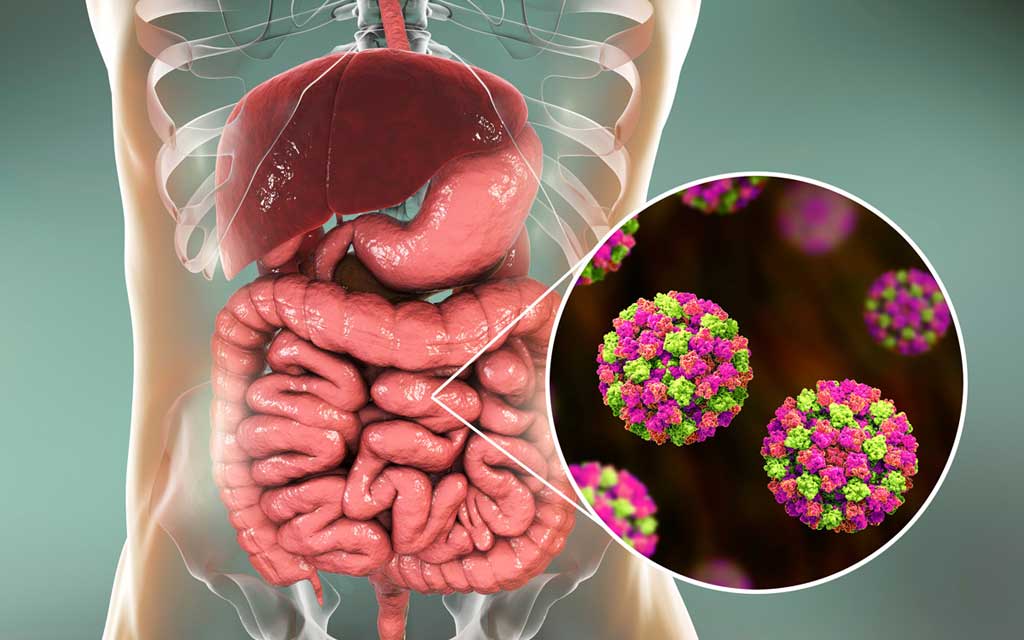 Image Source: Shutterstock
Image Source: Shutterstock Foodborne Illness Statistics
The CDC estimates that each year 48 million people get sick from a foodborne illness, 128,000 are hospitalized, and 3,000 die.
To prevent foodborne illness, it is necessary to understand how food becomes unsafe to eat and what proactive measures can be taken to keep food safe.
- Learn about foodborne pathogens, cross contamination, cold and hot food safety, and best practices to prevent foodborne illness.
- Food Manager ANSI Certification: $99.00 - Valid in all States
- Food Handler Training: Only $7.00!
- 10% OFF: Enter Promo Code "train10off" at Checkout
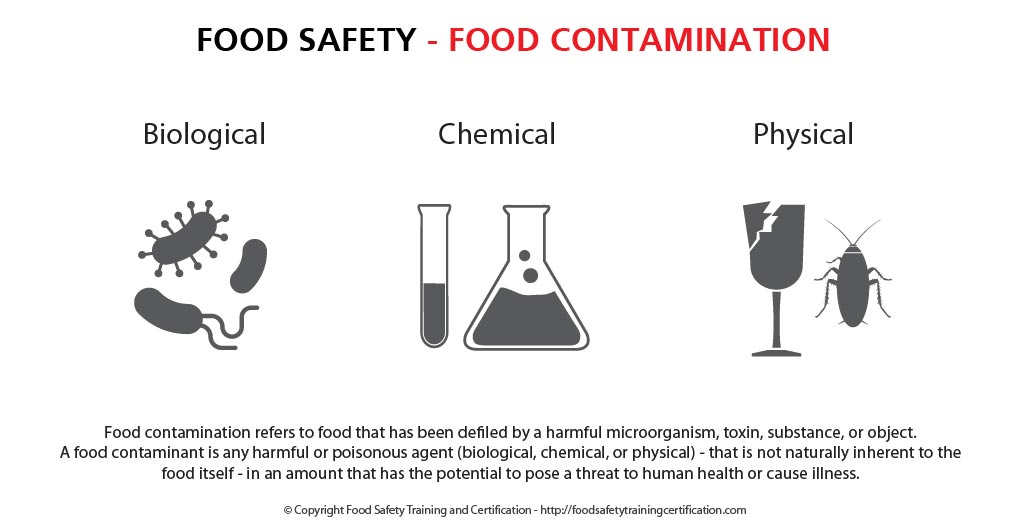
Food Hazards
A food hazard refers to any agent that has the potential to cause adverse health consequences for consumers. Food safety hazards occur when food is exposed to hazardous agents which result in contamination of that food. Food hazards may be biological, chemical, physical, or allergenic.
The causes of foodborne illness can fall into the following 3 categories:
- Biological hazards include bacteria, viruses, and parasites. Bacteria and viruses are responsible for most foodborne illnesses. Biological hazards are the biggest threat to food safety. They can be inherent in the product or due to mishandling (e.g., time/temperature abuse).
- Chemical hazards include natural toxins and chemical contaminants. Some natural toxins are associated with the food itself (i.e., certain mushrooms, PSP in molluscan shellfish), some are made by pathogens in the food when it is time/temperature abused (i.e., histamine development in certain seafood species). Some additives, such as sulfites, can be a hazard to some people. Chemical contamination can occur when products (i.e., cleaners) are not used correctly.
- Food allergens are a chemical hazard in the natural toxin sub-category. Some people are sensitive to proteins in foods. The 8 major food allergens include: milk, eggs, fish, crustacean shellfish (lobster, crab, shrimp), wheat, soy, peanuts, tree nuts.
- Physical hazards can include glass, metal, dirt, hair, droppings from pests can also cause foodborne illness. Sometimes, physical contaminants can also be biologically contaminated.
Bacteria Growth and Food
Given the right conditions, millions of bacteria can grow on common, everyday foods. These conditions are:
- Time and temperature: Bacteria grow most rapidly in the range of temperatures between 40 °F and 140 °F, doubling in number in as little as 20 minutes. This range of temperatures is often called the “Danger Zone.” So, it’s important not to keep food at this temperature for too long.
- Oxygen: Most bacteria require air to survive, these are called aerobic bacteria. Although some bacteria – called anaerobic bacteria – can survive without oxygen. Which is why it’s still possible to get food poisoning from canned food items.
- Food: Bacteria need a constant source of food to survive, especially protein. High protein foods such as meat are particularly vulnerable to biological contamination from bacteria, which means they’re considered high-risk foods. High-risk foods that bacteria love best include dairy products, meat, poultry, fish and shellfish
- Water: Water is essential to bacterial growth and without it, most bacteria will die. Which is why drying foods as a way of preservation are so effective and have been performed for thousands of years. This includes moisture in ‘wet’ foods such as juicy meats, sandwich fillings, soups, sauces and dressings.
- PH Levels: PH refers to food acidity and is measured on a scale of 1 (acidic) to 14 (alkaline). Most fruits generally have a PH level of between 1 – 5.9, so are considered acidic. While many alkaline foods such as vegetables have a PH level at the other end of the scale. Bacteria thrive in neutral foods that are neither acidic or alkaline and generally have a PH level of between 6 – 8.9. Foods such as meat and seafood are prime examples of neutral foods.
High Risk/Low Risk Foods for Bacterial Growth
High-risk foods are those that have ideal conditions for bacterial growth. This means they’re usually:
- Neutral in acidity
- High in starch or protein
- Moist
Examples: Foods such as raw meat or seafood, cooked rice or pasta, eggs, and dairy are all considered high-risk because they provide the perfect environment for bacteria to grow. This is why it’s essential to practice proper food handling when dealing with these foods.
 Image Source: Shutterstock
Image Source: Shutterstock Low-risk foods are those that don’t have particularly good bacterial growth conditions. These foods are:
- High in acidity
- High in salt or sugar
- Dried
- Canned or vacuum packed
Examples: Low-risk foods like dry goods, breakfast cereals, pickled foods, uncooked rice or pasta, and jams. Although these foods are not common sources of biological contamination, the appropriate care must still be taken when handling them.
Symptoms of Foodborne Illness
- Common symptoms of foodborne illness are diarrhea and/or vomiting, typically lasting 1 to 7 days. Other symptoms might include abdominal cramps, nausea, fever, joint/back aches, and fatigue.
- What some people call the “stomach flu” may actually be a foodborne illness caused by a pathogen (i.e., virus, bacteria, or parasite) in contaminated food or drink.
- The incubation period (the time between exposure to the pathogen and onset of symptoms) can range from several hours to 1 week.
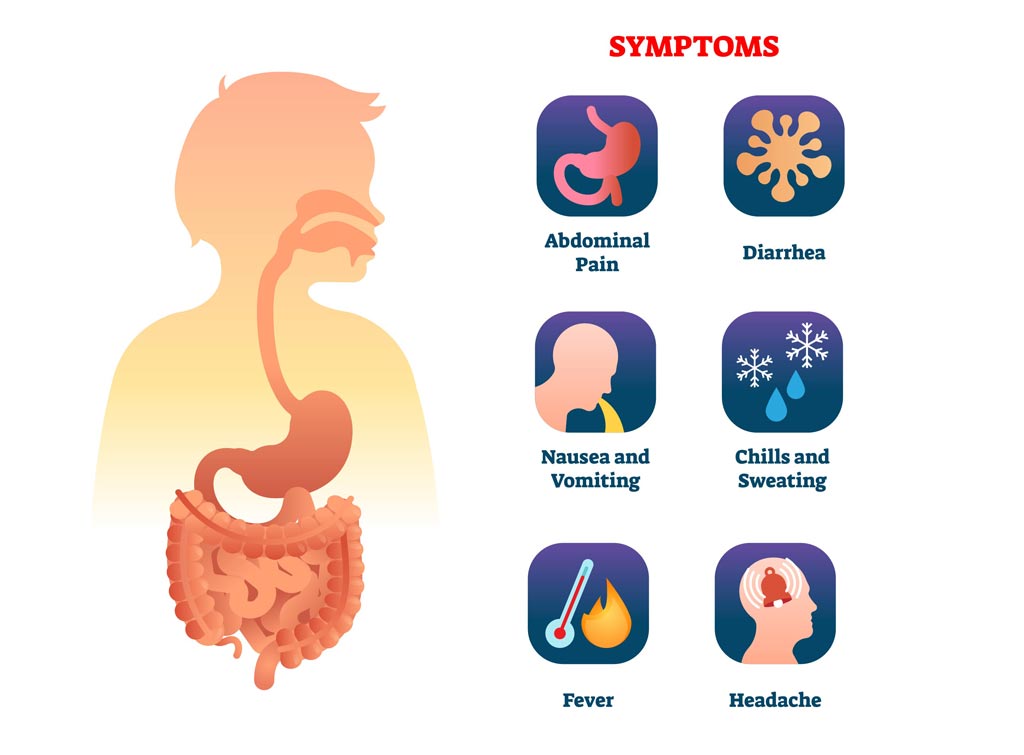 Image Source: Shutterstock
Image Source: Shutterstock People (Groups) Vulnerable to Foodborne Illness
Foodborne illness can affect anyone who eats contaminated food. However, certain populations are more susceptible to becoming ill with a greater severity of illness. These groups include:
- Pregnant women;
- Infants and young children;
- Older adults;
- People taking certain kinds of medications or with immune systems weakened from medical conditions, such as diabetes, liver disease, kidney disease, organ transplants, HIV/AIDS, or from receiving chemotherapy or radiation treatment.
Most people with a foodborne illness get better without medical treatment, but people with severe symptoms should see their doctor.
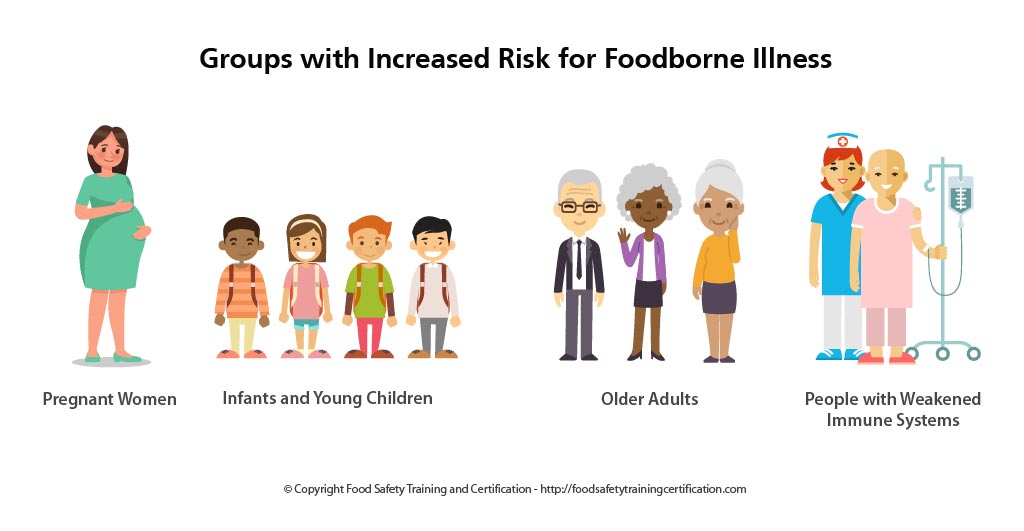
These vulnerable groups should take extra precautions and avoid the following foods:
- Raw or rare meat and poultry;
- Raw or undercooked fish or shellfish;
- Raw or undercooked eggs or foods containing them ( cookie dough and homemade ice cream);
- Fresh sprouts;
- Unpasteurized ciders or juices;
- Unpasteurized milk and milk products;
- Uncooked hot dogs.
Foodborne Disease-Causing Biological Organisms
The chart below includes foodborne disease-causing organisms that frequently cause illness in the United States.
| Organism | Onset Time After Ingesting | Signs & Symptoms | Duration | Food Sources |
|---|---|---|---|---|
| Bacillus cereus | 10-16 hrs | Abdominal cramps, watery diarrhea, nausea | 24-48 hours | Meats, stews, gravies, vanilla sauce |
| Campylobacter jejuni | 2-5 days | Diarrhea, cramps, fever, and vomiting; diarrhea may be bloody | 2-10 days | Raw and undercooked poultry, unpasteurized milk,contaminated water |
| Clostridium botulinum |
12-72 hours | Vomiting, diarrhea, blurred vision, double vision, difficulty in swallowing, muscle weakness. Can result in respiratory failure and death | Variable | Improperly canned foods, especially home-canned vegetables, fermented fish, baked potatoes in aluminum foil |
| Clostridium perfringens |
8–16 hours | Intense abdominal cramps, watery diarrhea | Usually 24 hours |
Meats, poultry, gravy, dried or precooked foods, time and/or temperature-abused foods |
| Cryptosporidium | 2-10 days | Diarrhea (usually watery), stomach cramps, upset stomach, slight fever | May be remitting and relapsing over weeks to months | Uncooked food or food contaminated by an ill food handler after cooking, contaminated drinking water |
| Cyclospora cayetanensis |
1-14 days, usually at least 1 week | Diarrhea (usually watery), loss of appetite, substantial loss of weight, stomach cramps, nausea, vomiting, fatigue | May be remitting and relapsing over weeks to months | Various types of fresh produce (imported berries, lettuce, basil) |
| E. coli (Escherichia coli) producing toxin |
1-3 days | Watery diarrhea, abdominal cramps, some vomiting | 3-7 or more days | Water or food contaminated with human feces |
| E. coli O157:H7 | 1-8 days | Severe (often bloody) diarrhea, abdominal pain and vomiting. Usually, little or no fever is present. More common in children 4 years or younger. Can lead to kidney failure. | 5-10 days | Undercooked beef (especially hamburger), unpasteurized milk and juice, raw fruits and vegetables (e.g. sprouts), and contaminated water |
| Hepatitis A | 28 days average (15-50 days) | Diarrhea, dark urine, jaundice, and flu-like symptoms, i.e., fever, headache, nausea, and abdominal pain | Variable, 2 weeks-3 months | Raw produce, contaminated drinking water, uncooked foods and cooked foods that are not reheated after contact with an infected food handler; shellfish from contaminated waters |
| Listeria monocytogenes |
9-48 hrs for gastro-intestinal symptoms, 2-6 weeks for invasive disease | Fever, muscle aches, and nausea or diarrhea. Pregnant women may have mild flu-like illness, and infection can lead to premature delivery or stillbirth. The elderly or immunocompromised patients may develop bacteremia or meningitis. | Variable | Unpasteurized milk, soft cheeses made with unpasteurized milk, ready-to-eat deli meats |
| Noroviruses | 12-48 hrs | Nausea, vomiting, abdominal cramping, diarrhea, fever, headache. Diarrhea is more prevalent in adults, vomiting more common in children. | 12-60 hrs | Raw produce, contaminated drinking water, uncooked foods and cooked foods that are not reheated after contact with an infected food handler; shellfish from contaminated waters |
| Salmonella | 6-48 hours | Diarrhea, fever, abdominal cramps, vomiting | 4-7 days | Eggs, poultry, meat, unpateurized milk or juice, cheese, contaminated raw fruits and vegetables |
| Shigella | 4-7 days | Abdominal cramps, fever, and diarrhea. Stools may contain blood and mucus. | 24-48 hrs | Raw produce, contaminated drinking water, uncooked foods and cooked foods that are not reheated after contact with an infected food handler |
| Staphylococcus aureus | 1-6 hours | Sudden onset of severe nausea and vomiting. Abdominal cramps. Diarrhea and fever may be present. | 24-48 hours | Unrefrigerated or improperly refrigerated meats, potato and egg salads, cream pastries |
| Vibrio parahaemolyticus |
4-96 hours | Watery (occasionally bloody) diarrhea, abdominal cramps, nausea, vomiting, fever | 2-5 days | Undercooked or raw seafood, such as shellfish |
| Vibrio vulnificus | 1-7 days | Vomiting, diarrhea, abdominal pain, bloodborne infection. Fever, bleeding within the skin, ulcers requiring surgical removal. Can be fatal to persons with liver disease or weakened immune systems. | 2-8 days | Undercooked or raw seafood, such as shellfish (especially oysters) |
Summary
It is very important to understand what, why, and how foods can make you sick, but more importantly, the food safe principles and procedures to prevent foodborne illnesses.
