Norovirus is a highly contagious virus and the most common viral foodborne illness. According to the CDC, every year in the U.S., norovirus leads to 71,000 hospitalizations and 800 deaths. Likewise, each year foodborne norovirus illness costs about $2 billion, mainly due to lost productivity and healthcare expenses.
Biological Foodborne Contamination
Food contamination refers to food that has been defiled by a harmful microorganism, toxin, substance, or object.
A food contaminant is any harmful or poisonous agent (biological, chemical, or physical) – that is not naturally inherent to the food itself – in an amount that has the potential to pose a threat to human health or cause illness.
- Learn about foodborne pathogens, cross contamination, cold and hot food safety, and best practices to prevent foodborne illness.
- Food Manager ANSI Certification: $99.00 - Valid in all States
- Food Handler Training: Only $7.00!
- 10% OFF: Enter Promo Code "train10off" at Checkout
Because food becomes hazardous by contamination, food contaminants are also referred to as food hazards. A hazard is any source of potential damage, harm, or adverse health effects on something or someone.
Biological food hazards are biological agents that can pose a threat to human health. Biological hazards are the main causes of foodborne illness.
Biological food hazards are also called foodborne pathogens – or infectious organisms that are capable of causing human disease. These pathogenic organisms include bacteria, viruses, and parasites. With the exception of certain parasites, most biological foodborne pathogens are microscopic.
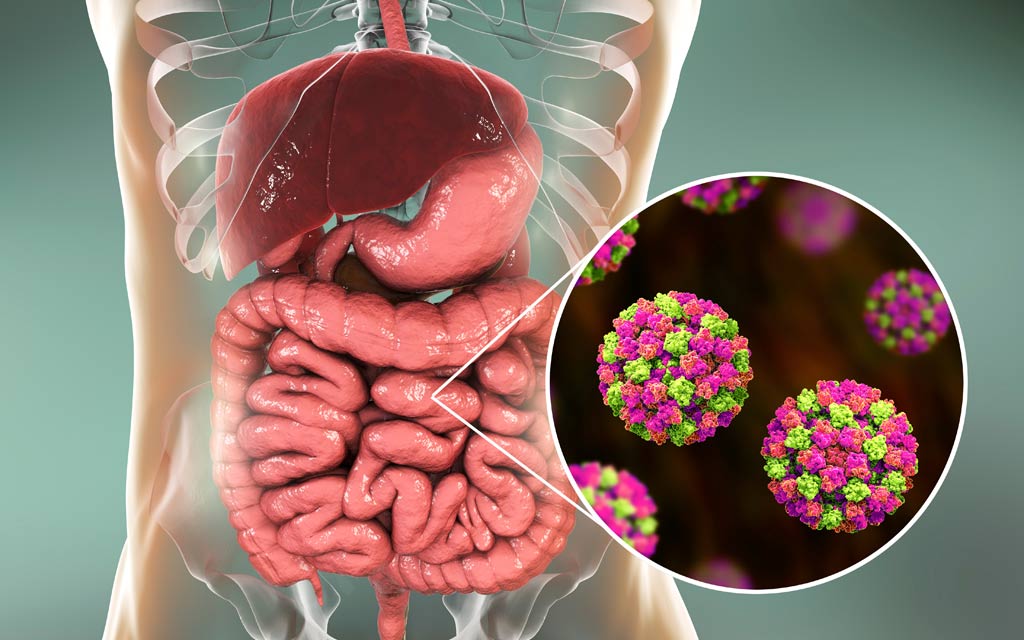
How do people become infected with Norovirus?
Anyone can get norovirus. Young children, the elderly, and anyone who already has other illnesses may experience longer, more serious illness, and rarely, even death.
 Image Source: Shutterstock
Image Source: Shutterstock Only a few norovirus particles can make people sick and the infection can be acquired a few different ways:
- Consuming water – or produce (fruit and vegetables) irrigated with water – contaminated with human or animal feces.
- Consuming shellfish (oysters, clams, mussels, scallops), crustaceans (shrimp, crabs, and lobsters), and their products – that are farmed or harvested in water contaminated with human sewage.
- Consuming food handled by a person infected with the virus – or an uninfected person transfers the virus to food with contaminated hands.
- In direct contact with an object, surface, or person that has been infected with the virus and then touches their nose, mouth, or eyes.
Symptoms of Norovirus Infection
Symptoms of norovirus infection typically begin 12 to 48 hours after exposure, last for 1 to 3 days, and cause acute gastroenteritis (diarrhea, vomiting, and abdominal pain) along with fever, headache, and body aches.
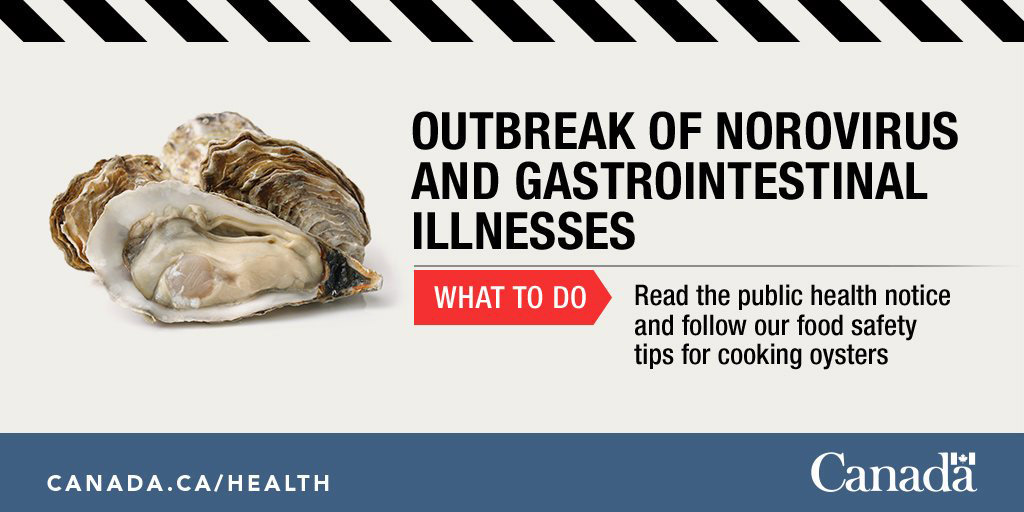
2018 Contaminated Oyster Norovirus Outbreak
The FDA reported a 2018 multi-state outbreak of Norovirus illnesses that was associated with contaminated oysters harvested in Baynes Sound, British Columbia, Canada, and were distributed to AK, CA, FL, HI, IL, MA, NY, and WA. The contamination was determined to be human sewage in the marine environment.
According to the the Public Health Agency of Canada, a total of 176 cases of gastrointestinal illness linked to oyster consumption were reported in three provinces: British Columbia (137), Alberta (14), and Ontario (25). No deaths were reported. Individuals became sick between mid-March and mid-April 2018.
The California Department of Public Health (CDPH) reported approximately 100 individuals reported illness after they consumed raw British Columbian oysters sold by restaurants and retailers throughout the state.
Although the outbreak appears to be over, this outbreak is a reminder that oysters are a known risk for causing food-related illness if consumed as a raw product.
Outbreak of norovirus and gastrointestinal illnesses linked to raw oysters – August 1, 2018 – Final Update
Norovirus Prevention – How can I stay safe?
Because norovirus is highly contagious, infection outbreaks occurs most frequently in closed and crowded environments such as restaurants, hospitals, nursing homes, child care centers, schools and cruise ships.
Maintaining good hygiene is the first line of defense. In addition to washing with soap and water after using the bathroom or eating, it is also recommended using alcohol-based sanitizers as an additional safety measure.
Follow these tips to reduce your chances of getting a norovirus infection:
- Don’t eat raw or undercooked oysters or other shellfish. Fully cook them before eating, and only order fully cooked oysters at restaurants.
- Safe cooking and food preparation is also essential – by thoroughly disinfecting kitchen surfaces, washing all produce, and cooking all food to adequate temperatures.
- Separate cooked seafood from raw seafood and its juices to avoid cross contamination.
- Wash your hands with soap and water after handing raw seafood.
- Cover any wounds if they could come into contact with raw seafood or raw seafood juices or with brackish or salt water.
- Wash open wounds and cuts thoroughly with soap and water if they have been exposed to seawater or raw seafood or its juices.
References
- Centers for Diseases prevention and Control (CDC) – Norovirus
https://www.cdc.gov/norovirus/trends-outbreaks/burden-US.html - Mayo Clinic – Noroviros Infection
https://www.mayoclinic.org/diseases-conditions/norovirus/symptoms-causes/syc-20355296 - CDC – Food Safety
https://www.cdc.gov/foodsafety/foodborne-germs.html - U.S. FDA – Foodborne Illnesses
https://www.fda.gov/food/consumers/what-you-need-know-about-foodborne-illnesses - U.S. FDA – Foodborne Pathogens
https://www.fda.gov/food/outbreaks-foodborne-illness/foodborne-pathogens - FDA – Fish and Fishery Products Hazards and Controls Guidance
https://www.fda.gov/food/seafood-guidance-documents-regulatory-information/fish-and-fishery-products-hazards-and-controls-guidance-4th-edition